Refer also to the bpac publication:
Obstructive sleep apnoea in adults(external link)
Obstructive sleep apnoea (OSA) is a condition characterised by loud snoring, episodes of sleep related upper airway obstruction and daytime sleepiness. The obstruction may be complete, leading to cessation of airflow (apnoea) or partial, leading to a markedly reduced inspiratory flow (hypopnoea).
OSA can be defined as the presence of five or more obstructive events (either apnoeas or hypopnoeas) per hour of sleep i.e. Apnoea-Hypopnoea Index (AHI) of 5 or more. Elevation in the AHI can occur (especially if mild) without daytime sleepiness.
The obstructive sleep apnoea syndrome is defined as the presence of OSA with daytime sleepiness. During apnoeas and hypopnoeas the difficulty in inspiration causes repeated arousals from sleep. Poor quality of sleep is then the cause of daytime sleepiness. OSA is both common and under-diagnosed.
Excessive daytime sleepiness, difficulty in concentration, an increased rate (2-5 times) of road traffic accidents and impairment of skilled motor tasks are consistently associated with moderate and severe OSA. Applicants often only recognize the extent of their performance decrement once it is successfully remedied with treatment. The diagnosis is made with evaluation in a sleep clinic.
OSA is also associated with an increased risk of coronary artery disease, hypertension, stroke and diabetes although there is some debate as to whether the association is causal or secondary to associated obesity, which is often present. Because of this association, it is appropriate to also conduct a cardiovascular risk assessment.
Risk factors for OSA include increasing age, obesity, hypothyroidism and a family history of OSA. Type 2 diabetes is found in association with OSA, probably secondary to the frequently present obesity. Most patients seen in a sleep clinic are significantly overweight, although not all with around 40% of OSA being attributable to maxillofacial factors (particularly retrognathia). The majority with significant OSA snore to a level that is commented on by their bed partners, who typically report being alarmed by the apnoeic episodes. Specific questions addressed to the partner can be helpful if the medical examiner suspects that OSA may be an issue. Of note a few individuals with severe OSA move so little air before they obstruct that they do not snore as much as those with a less severe condition. However, they may have a history of severe snoring which has subsequently lessened. Severe snoring is a sensitive marker for OSA. Daytime sleepiness as a symptom is also reasonably sensitive, but may not be declared to a ME unless specific questions are asked.
There is also a group who despite having significant OSA state that they are not at all sleepy during the day and have very low Epworth scores, i.e. 0 – 3 (normal maximum score is about 9). In this setting an objective measure of the individual’s ability to maintain wakefulness may be helpful (Maintenance of wakefulness test).
There is a separate but related condition that is not uncommon. A patient may have a history of severe snoring. However, on sleep studies, there is no evidence of OSA but the patient is sleepy during the day and responds well to continuous positive airway pressure (CPAP). This condition is known as the 'upper airway resistance syndrome'.
CPAP is very effective in those who tolerate it. Most patients who are symptomatic, are accurately assessed and who have proper fitting of their interface (mask and headset), tolerate CPAP well. Technological advancements include: Humidification which reduced adverse upper airway side-effects; PAP devices that can auto-titrate (APAP) to maintain an open airway at the lowest effective pressure; expiratory pressure relief or C-Flex that lower pressure in the first part of expiration; downloadable compliance and AHI data.
In the one third of patients that do not tolerate CPAP, a mandibular advancement device (MAD) may be considered. Predictors of MAD success include: good dentition and nasal airflow; ability to protrude the mandible; lower BMI (< 35kg/m2) and positional OSA. Be aware that some changes in bite (occlusion) occur in most long term MAS treated patients so a dentist needs to be involved in follow-up. Upper airway surgery can be considered in selected patients if CPAP and MAS treatment unsuccessful. This usually requires a Respiratory / Sleep Specialist opinion.
The Epworth sleepiness scale is a subjective measure of daytime sleepiness that numerically scores the response to eight questions concerning an individual’s likelihood of sleeping during different activities e.g. watching television, sitting and talking to someone. First published in 1991 and named after the Sleep Disorders Unit, Epworth Hospital, Melbourne, Australia. Copyright of Murray W. Johns, Australian physician, 1937.
It can be useful to get the spouse to participate in completion of this questionnaire. It is not flight task specific and is easily manipulated so low / normal values in the context of employment cannot be relied upon to exclude a diagnosis of aeromedically significant OSA. The Epworth questionnaire should be interpreted with caution.
ICAO recommends that the diagnosis of OSA should be considered in crew members who are overweight, have Type 2 diabetes, have a history of snoring or complain of excess daytime sleepiness. Any pilot who has fallen asleep on the flight deck, outside a planned rest period, may need investigation. Fatigue, shift work, sleep restriction and task monotony need to be considered as potential contributing factors.
Applicants who have hypertension and those with certain facial features, such as retrognatism, crowded pharynx, tonsil hypertrophy etc, should also be considered for this diagnosis. People with a BMI of 35 or more have a ~ 70-75 % likelihood of suffering from OSA and those with a BMI of 40 or above, a ~ 80% likelihood of having OSA.
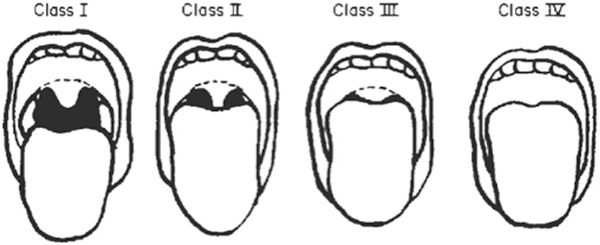
The Mallampati score, initially used in anaesthesia to predict difficulties with intubation also predicts OSA. A Grade III or IV suggests the presence of OSA (AHI >5) but does not predict for severe OSA (AHI >30). However a high Mallampati score should incite the ME to inquire further about OSA.
| Grade I: | Entire tonsil clearly visible |
| Grade II: | Upper half of tonsil fossa visible |
| Grade IV: | Soft and Hard Palate clearly visible |
| Grade V: | Only Hard Palate visible |
Obstructive sleep apnoea is not the only cause of daytime hypersomnolence. Shift work related sleep restriction, periodic leg movement disorder, narcolepsy, idiopathic hypersomnolence, sleep phase reversal, poor sleep hygiene and sleep disturbance due to depression or pain should be considered in patients who have hypersomnolence but normal respiratory sleep studies. Sleepy individuals require evaluation, even in the absence of OSA risk factors.
The ME should inquire about snoring at a level that disturbs someone sleeping in the same room, tendency to fall asleep or doze at inappropriate times and traffic accidents.
The ME should consider the BMI, neck circumference, blood pressure, glucose metabolism status and facial and throat morphologic features of the applicant. The ME should also inquire about alcohol consumption.
An Epworth Sleepiness questionnaire should be completed in case of any suspicion of OSA. It is however worth noting that, in the context of employment medical examinations and the regulatory environment, the Epworth Sleepiness questionnaire has a poor negative predictive value. A score of 10 or above has however a high predictive value for OSA.
bpac advises: Flemmons’ score (adapted from Skjodt, 2008)
Measured neck circumference + Addition as below = Adjusted neck circumference
Neck circumference in cm + add:
3 cm for snoring history
3 cm for history of witnessed apnoea
4 cm for a history of hypertension
| Result | OSA risk |
| < 43 cm | Low risk (17% probability) |
| 43 – 47.9 cm | Intermediate risk |
| 48 cm and above | High risk (> 80 %) |
Level 1 study: This is a Polysomnography conducted in a laboratory with a technician present and under the supervision of a respiratory physician involved in sleep medicine. This is the gold standard.
Level 2 study: This is an unattended sleep study, recording the same parameters. The patient is pre-wired in the lab or a technician may attend the patient at home to conduct the study there. This has the advantage of a more natural environment, but the study is not witnessed.
Level 3 study: Records airflow, respiratory effort, SatO2 and heart rate. It is inadequate for certification purpose.
Level 4 study: typically only records SatO2 and heart rate. It is inadequate for certification purpose.
Once satisfactory CPAP/APAP treatment is established, demonstrated by CPAP Log, reduced daytime sleepiness and absence of snoring on treatment, a return to flying should normally be allowed. Unless major weight loss occurs, CPAP/APAP or MAD treatment is likely to be needed lifelong. Follow-up at a sleep clinic may be required to ensure the ongoing adequacy of treatment and compliance.
An applicant with demonstrated Obstructive Sleep Apnoea should be considered as having a condition of aeromedical significance unless:
An applicant treated by other means or not fulfilling the above criteria should be considered has having a condition that is of aeromedical significance and be assessed via the flexibility process.
In doubt the Medical Examiner should consult with CAA.